Scientific Concept and Goals

Cardiovascular disease (CVD) is the leading cause of death worldwide.
According to the World Health Organization (WHO), at least half of the deaths and disabilities resulting from CVD could be avoided by improved primary or secondary prevention. Improved prevention of CVD requires a better understanding of the pathomechanisms and a faster and more efficient translation of novel leads into clinical application.
Therefore, to effectively decrease CVD mortality, an integrated approach is needed that includes both prevention of the establishment of CVD via primary preventive measures and therapeutic targeting of established CVD with manifest vascular and myocardial damage.
The mission of the Munich Heart Alliance is to accelerate the development of strategies to prevent and treat CVD. To fulfill this mission, we will focus on the following scientific objectives, each addressed by a distinct research program:
I) to identify, on a population level, risk factors predisposing to CVD
II) to model CVD in order to dissect the underlying mechanisms
III) to develop novel therapeutic strategies against CVD

Example Subtitle
Example Title
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Mauris tempus nisl vitae magna pulvinar laoreet. Nullam erat ipsum, mattis nec mollis ac, accumsan a enim. Nunc at euismod arcu. Aliquam ullamcorper eros justo, vel mollis neque facilisis vel.
Predisposition and Risk
The aim of the research program Predisposition and Risk is to determine factors that predispose to a particular phenotype (such as plaque formation, infarction or restenosis) and to provide parameters of cardiovascular disease (CVD) risk.
These risk factors can then be used to stratify study populations and to predict disease-related events. For a successful translation of such epidemiologic research into benefits for at-risk-individuals and patients we set emphasis on the following research topics:
- the characterization of additional CVD-related phenotypes based on imaging, genetic and metabolic profiling and response to treatment
- the identification of critical time points in the dynamic development of CVD by repeated measurements within individuals as provided by cohort studies
- the investigation of comprehensive datasets from disease-related tissues other than blood, specifically from multiple tissues and the use of cell lines including iPS technology
Within this research program the ability and position to take part in international large-scale epidemiological studies is expanded.
Recent advances in genomic medicine have led to the identification of a large number of genes that harbor variations contributing directly or indirectly to coronary heart disease and its associated conditions such as arrhythmias, heart failure or stroke. Researchers from the Munich Heart Alliance contribute continuously to the identification of new genes and innovative metabolomic studies have been successful in correlating genetic variations with metabolomic profiles. Further emphasis is set on such studies as this will lead to the identification of novel therapeutic targets.
A comprehensive assessment of risk factor profiles in combination with molecular and clinical phenotyping and their integration into further individualized risk stratification makes an interdisciplinary approach mandatory. The research network within the Munich Heart Alliance provides an ideal basis for this. Researchers of the MHA have exceptional expertise in assessing the impact of physical activity and nutrition on CVD. Within this program aspects of primary and secondary prevention of CVD will be addressed as well as factors of survival by integrating clinical, epidemiological, health services research and health economics. Novel approaches will be developed to integrate physical activity, mental health and environmental exposures as well as genetic, proteomic and metabolic markers for predicting susceptibility to CVD.
Disease Modeling
A critical prerequisite for successful translation to human application is the modeling of cardiovascular disease (CVD) as a complex disease in relevant systems.
Munich Heart Alliance network a broad range of established and ongoing in vitro and in vivo models - comprising patient-specific induced pluripotent stem cells as well as small and large animal models - is available. The focus in this research program will be on vascular inflammation and remodeling as well as on platelet biology.
The chronic inflammatory response of the arterial wall hallmarks both early and late stages of CVD. The inhibition of the recruitment of immune cells to the arterial vessel wall could therefore be a promising strategy to treat and prevent CVD. One goal of the Munich Heart Alliance is to identify and target processes that are specifically related to vascular inflammation in CVD and develop drug candidates without adverse immunological effects.
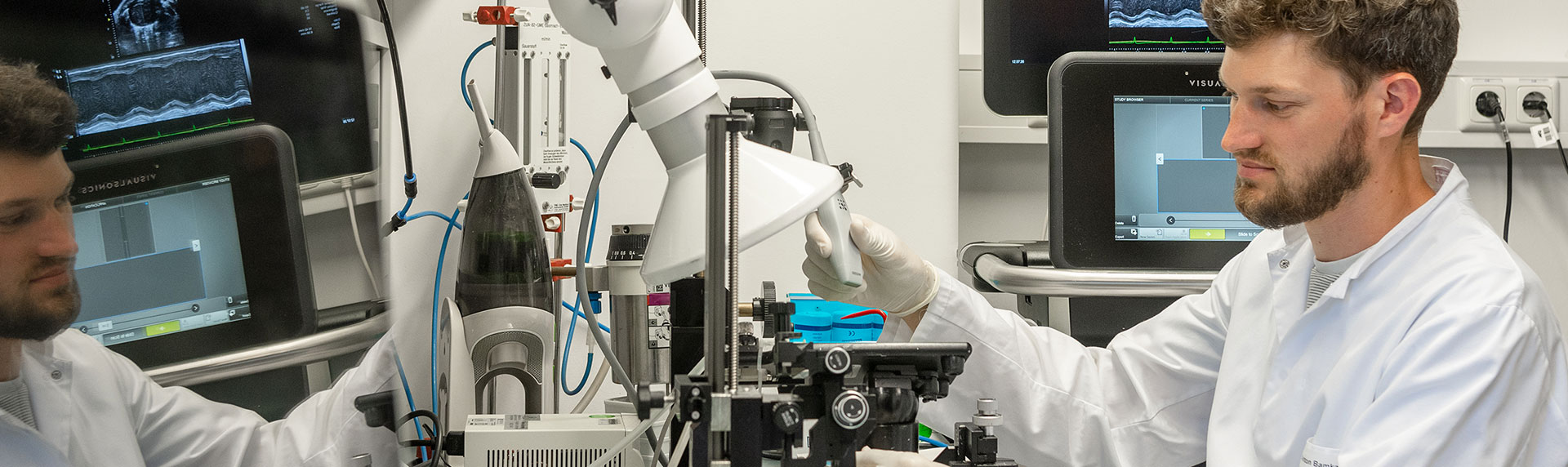
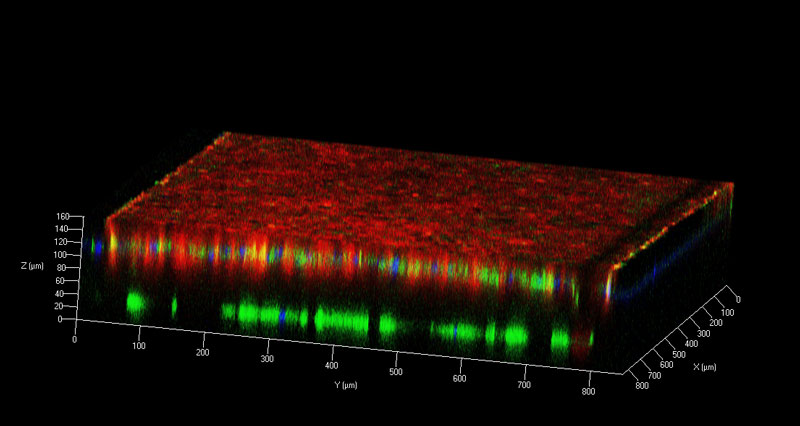
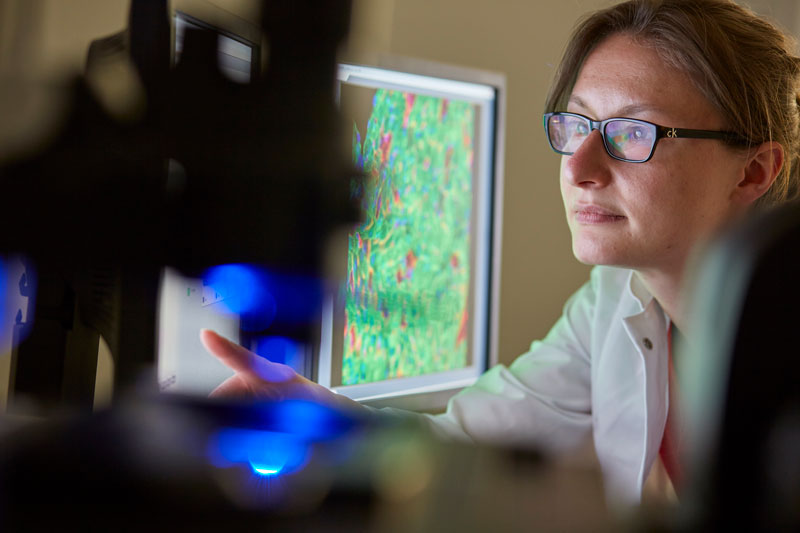
We characterize inflammatory responses on a cellular level by novel imaging approaches and dissect mechanisms underlying remodeling and microcirculatory disturbances. Advanced intravital microscopy is employed to address the question to what extent impairment of microcirculatory blood flows affects development or progression of macrovascular disease.
Dysregulation of thrombosis and haemostasis are considered key events both in the manifestation of advanced CVD and also in the initiation of the atherosclerotic process itself. While efficient anti-thrombotic strategies have been integrated into daily clinical management of CVD patients, these approaches are non-specific since they also target normal haemostasis and hence are associated with considerable bleeding complications. To develop novel strategies that prevent atherothrombosis at minimized effects on normal haemostasis, one of the major challenges of MHA research network is to gain a better understanding of the molecular and cellular mechanisms underlying thrombotic complications of CVD.

Novel Therapeutic Strategies
Research within this program aims to bring the wealth of novel targets to clinical application as well as to define new indications for known drugs.
The focus is set on the development of therapies that interfere with CVD-induced vascular and myocardial damage.
The new generation of drug-eluting stents (DES) has drastically improved the management of patients with cardiovascular disease (CVD). Currently, all DES patients are uniformly treated with a protracted dual anti-platelet (DAP) therapy. However, the current DAP therapy impairs also normal hemostasis and may cause severe bleeding complications. Therefore, a major task of the Munich Heart Alliance is to develop strategies that prevent CVD manifestation and/or progression without compromising essential processes such as immune defense, vascular healing and arrest of bleeding.
One focus will be on the evaluation of novel stent designs with improved anti-proliferative, pro-healing and anti-inflammatory characteristics. A second major focus will be to develop and evaluate novel antithrombotic strategies that interfere with platelet adhesion and/or coagulation in diseased (or stented) coronary arteries but have a minor effect on normal hemostasis. New antithrombotic concepts will be evaluated by Munich Heart Alliance members in phase I/II trials and in the large phase III/IV ISAR BRAVE and the ISAR REACT trials.
Cardiac fibrosis is a key structural alteration of post myocardial infarction and a critical element of cardiac remodeling and of cardiac arrhythmias.
In a preclinical study, scientists of the Munich Heart Alliance have recently shown that interfering with a cardiac fibroblast-specific signaling mechanism (miR-21-mediated control of fibroblast ERK activity) prevents and even cures structural and functional deterioration in a mouse model of cardiac damage. This study represents the first example of microRNA therapeutics in a cardiovascular disease model and suggests a new therapeutic entry point for cardiac disease. Based on this expertise, the Munich Heart Alliance aims to employ RNA-based therapeutics to target cardiac fibrosis to cure myocardial infarction-induced myocardial damage and arrhythmias. An especially powerful facet of microRNA biology is the ability of individual microRNAs encoding proteins with related functions (e.g. cell growth, contractility, etc.), in contrast to classical drugs, which act on specific cellular targets.
Despite the general improvement in outcomes among survivors of acute myocardial infarction the rate of death remains highest in the weeks after the event. Sudden cardiac death accounts for approximately 20-50% of all deaths in this population. Combining the expertise of partners of the Munich Heart Alliance we aim to improve the prevention of sudden cardiac death on post myocardial infarction patients by testing a novel strategy for implantable cardioverter-defibrillator therapy for the reduction of total mortality in a large-scale prospective randomized trial.
The MHA bioimaging expertise is essential for all of the above efforts to monitor the proposed translation of new therapeutic concepts into clinical application. Within the Munich research area, scientists have focused on developing imaging methods to assess the beneficial effect of cardiovascular interventions (myocardial perfusion, infarct size, area of risk etc.). Current imaging research addresses the quantitative visualization of biological processes in order to longitudinally evaluate the natural history of disease and its modification by therapeutical interventions.